Total Protein Test 01797522136
Introduction
Laboratory investigations play a crucial role in modern medical diagnosis and patient management. Among the many biochemical tests used in clinical pathology, the Total Protein Test is one of the most fundamental and informative blood tests. It provides essential information about a patient’s nutritional status, liver function, kidney function, immune health, and overall metabolic condition.

At HRTD Medical Institute, Dhaka, we emphasize in-depth theoretical knowledge combined with practical laboratory training to help students and healthcare professionals understand and correctly interpret essential diagnostic tests such as the Total Protein Test. This comprehensive guide explains the principles, clinical significance, methodology, interpretation, and real-life applications of the Total Protein Test in clinical practice.
What Is the Total Protein Test?
The Total Protein Test measures the total concentration of proteins present in blood serum or plasma. Proteins are vital macromolecules that perform numerous physiological functions, including:
- Maintaining osmotic pressure
- Transporting hormones, enzymes, and drugs
- Supporting immune defense
- Facilitating tissue repair and growth
The total protein level is mainly composed of two major fractions:
- Albumin
- Globulins
Together, these proteins reflect the body’s overall protein balance and metabolic state.

Types of Proteins Measured
1. Albumin
Albumin is the most abundant protein in blood plasma. It is synthesized in the liver and plays a key role in:
- Maintaining oncotic pressure
- Transporting substances such as bilirubin, calcium, hormones, and drugs
- Serving as a marker of liver function and nutritional status
2. Globulins
Globulins are a diverse group of proteins that include:
- Immunoglobulins (antibodies)
- Transport proteins
- Enzymes
- Complement proteins
Globulins are primarily involved in immune responses and inflammation.
Why Is the Total Protein Test Important?
The Total Protein Test is clinically significant because it helps detect, diagnose, and monitor various medical conditions, including:
- Liver diseases
- Kidney disorders
- Malnutrition
- Chronic infections
- Autoimmune diseases
- Plasma cell disorders such as multiple myeloma
At HRTD Medical Institute, students are trained to understand how abnormal protein levels can be early indicators of serious underlying diseases.

Normal Reference Range of Total Protein
The normal reference range may vary slightly depending on laboratory methods, but generally:
- Total Protein (Adults):
6.0 – 8.3 g/dL (60 – 83 g/L)
Reference ranges may differ based on age, sex, and physiological conditions.
Indications for Total Protein Test
A physician may order a Total Protein Test for the following reasons:
- Routine health check-up
- Unexplained weight loss
- Chronic fatigue
- Edema (swelling)
- Suspected liver or kidney disease
- Chronic infection or inflammation
- Monitoring nutritional status
- Suspected immunological disorders
Specimen Requirements
Sample Type
- Venous blood
Specimen
- Serum (preferred)
- Plasma (acceptable with certain anticoagulants)
Patient Preparation
- Usually no fasting required
- Fasting may be advised when combined with other tests
Principle of Total Protein Estimation
Several methods are used for measuring total protein, but the most common is the Biuret Method.
Biuret Method Principle
- Proteins react with copper ions in an alkaline solution
- This reaction forms a violet-colored complex
- The intensity of the color is directly proportional to the protein concentration
- Measured using a spectrophotometer
At HRTD Medical Institute, students receive hands-on laboratory training to perform the Biuret method accurately.
Other Methods of Total Protein Estimation
- Lowry Method
- Kjeldahl Method
- Refractometry (less accurate)
- Dye-binding methods
Among these, the Biuret Method is most widely used in clinical laboratories.
Procedure Overview (Biuret Method)
- Prepare reagents and calibrators
- Add serum sample to Biuret reagent
- Incubate at room temperature
- Measure absorbance using a spectrophotometer
- Calculate total protein concentration
Clinical Interpretation of Results
High Total Protein (Hyperproteinemia)
Causes include:
- Dehydration
- Chronic infections (e.g., tuberculosis)
- Multiple myeloma
- Chronic inflammatory conditions
- Liver diseases with increased globulin production
Low Total Protein (Hypoproteinemia)
Causes include:
- Malnutrition
- Liver failure
- Nephrotic syndrome
- Malabsorption syndromes
- Severe burns
- Chronic diarrhea
Albumin/Globulin (A/G) Ratio
The Total Protein Test is often interpreted along with the Albumin/Globulin ratio, calculated as:
A/G Ratio = Albumin ÷ Globulin
Normal A/G Ratio
- 1.0 – 2.2
An abnormal A/G ratio can indicate liver disease, kidney disease, or immune disorders.
Role of Total Protein Test in Liver Disease
In liver disorders:
- Albumin levels decrease due to impaired synthesis
- Globulin levels may increase due to chronic inflammation
- Total protein may appear normal or low
Understanding this pattern is essential for accurate diagnosis, and it is thoroughly taught at HRTD Medical Institute.
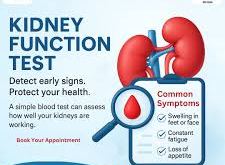
Role in Kidney Disease
In kidney diseases such as nephrotic syndrome:
- Excess protein is lost in urine
- Serum total protein and albumin decrease
- Leads to edema and fluid imbalance
Total Protein Test in Nutritional Assessment
Total protein measurement helps assess:
- Protein-energy malnutrition
- Chronic starvation
- Malabsorption disorders
It is especially important in hospitalized patients and elderly individuals.
Total Protein Test in Immune Disorders
In conditions like:
- Multiple myeloma
- Chronic infections
- Autoimmune diseases
Globulin levels rise, leading to increased total protein.
Limitations of Total Protein Test
- Does not identify individual protein fractions
- Cannot replace electrophoresis
- Influenced by hydration status
- Must be interpreted with clinical findings
Total Protein Test vs Serum Protein Electrophoresis
| Feature | Total Protein Test | Protein Electrophoresis |
|---|---|---|
| Measures | Total protein amount | Individual protein fractions |
| Cost | Low | Higher |
| Usage | Screening | Diagnostic confirmation |
Importance in Clinical Pathology Education
At HRTD Medical Institute, Dhaka, the Total Protein Test is an essential part of:
- Diploma in Pathology
- Medical Laboratory Technology courses
- Internship training programs
Students gain:
- Theoretical understanding
- Practical laboratory experience
- Result interpretation skills
- Clinical correlation knowledge
Quality Control in Total Protein Testing
Quality assurance includes:
- Use of control sera
- Calibration of instruments
- Proper reagent storage
- Regular maintenance of equipment
HRTD Medical Institute emphasizes strict laboratory quality control standards.
Common Errors and Precautions
- Hemolyzed samples may affect results
- Lipemic samples can interfere with absorbance
- Incorrect reagent preparation
- Improper calibration
Career Scope for Students Learning Total Protein Testing
Students trained at HRTD Medical Institute can work as:
- Medical Laboratory Technologists
- Clinical Pathology Assistants
- Diagnostic Lab Officers
- Hospital Lab Technicians
Why Learn Clinical Biochemistry at HRTD Medical Institute?
- Experienced faculty
- Modern laboratory facilities
- Hands-on training
- Industry-relevant curriculum
- Internship opportunities
- Strong career guidance
Conclusion
The Total Protein Test is a fundamental diagnostic investigation that provides valuable insights into liver function, kidney health, immune status, and nutritional balance. Accurate performance and correct interpretation of this test are essential skills for medical laboratory professionals.
At HRTD Medical Institute, Dhaka, students are trained to master both the scientific principles and clinical applications of the Total Protein Test. With a strong focus on quality education and practical exposure, HRTD Medical Institute continues to produce skilled pathology professionals for Bangladesh’s healthcare system.
Total protein test
A total protein test measures the overall protein levels (albumin and globulin) in your blood, assessing liver/kidney function, nutrition, and inflammation, often done with a blood draw as part of routine checkups or for unexplained symptoms like fatigue or swelling. High or low levels can signal issues with liver or kidney disease, malnutrition, infections, or immune problems, with results helping doctors diagnose and monitor various health conditions.
What it measures
- Albumin: Made by the liver, it prevents fluid leakage from vessels and carries substances.
- Globulin: Includes antibodies (immune function) and transport proteins.
- A/G Ratio: Compares albumin to globulin, providing more insight into specific issues.
Why it’s done
- Routine checkup: As part of general health screening.
- Diagnose conditions: To investigate liver or kidney disease, malnutrition, or autoimmune disorders.
- Monitor health: To track treatment for conditions affecting protein levels.
- Investigate symptoms: For unexplained weight loss, fatigue, or swelling.
How to prepare
- Follow fasting instructions if it’s part of a larger panel.
- Inform your doctor about all medications and supplements.
- Stay hydrated.
What results mean
- High levels: May indicate dehydration, inflammation, infection, or multiple myeloma.
- Low levels: Can point to malnutrition, liver disease (like cirrhosis), kidney disease, or digestive issues.
- An abnormal A/G ratio can suggest specific liver or immune problems.
Albumin
Albumin is a vital, water-soluble protein produced by the liver that constitutes about 50% of plasma protein, essential for maintaining oncotic pressure (preventing fluid leakage from blood vessels), transporting hormones, drugs, and nutrients throughout the body. Normal serum levels are 3.5–5.5 g/dL, with low levels indicating liver/kidney disease or malnutrition.
Key Functions and Characteristics
- Oncotic Pressure: Responsible for 75–80% of the plasma’s total colloid osmotic pressure.
- Transport: Binds and carries calcium, fatty acids, bilirubin, thyroxine, and pharmaceuticals.
- Synthesis: Produced in the liver at a rate of 10–15g per day.
- Distribution: Roughly 40% is in the bloodstream, with 60% in the extravascular space.
Clinical Significance
- Albumin Test: Measures levels in blood or urine (albuminuria) to assess kidney/liver health.
- Low Levels (Hypoalbuminemia): Caused by liver disease (cirrhosis), kidney disease, malnutrition, inflammation, or severe burns.
- High Levels (Hyperalbuminemia): Typically results from dehydration.
- Therapeutic Use: Administered intravenously (5% or 25% solutions) for volume expansion in shock, burns, and liver surgery.
Normal Ranges
- Adults: 3.4–5.4 g/dL (34–54 g/L).
- Children: 4.0–5.9 g/dL
Hypoalbuminemia
Hypoalbuminemia is a condition characterized by abnormally low levels of albumin—a crucial protein produced by the liver—in the blood (typically < 3.5 g/dL). It commonly arises from chronic inflammation, kidney disease, liver cirrhosis, or malnutrition, resulting in fluid leakage from blood vessels, leading to edema (swelling), fatigue, and ascites.
Key Aspects of Hypoalbuminemia
- Definition: Albumin is essential for maintaining osmotic pressure (keeping fluid in blood vessels) and transporting substances like hormones, drugs, and vitamins.
- Causes:
- Decreased production: Liver diseases (cirrhosis, hepatitis).
- Increased loss: Kidney damage (nephrotic syndrome), gastrointestinal losses (protein-losing enteropathy), or severe burns.
- Inflammation/Catabolism: Sepsis, injury, or severe infection.
- Symptoms: Edema in the legs, face, or abdomen (ascites), profound fatigue, muscle weakness, and, in severe cases, difficulty breathing.
- Diagnosis: Measured via a blood test (serum albumin test), often ordered as part of a liver function panel.
- Treatment: Primarily focuses on treating the underlying cause, rather than directly replacing albumin, which is rarely indicated.
Prognostic Significance
Hypoalbuminemia is a strong indicator of poor prognosis in hospitalized and critically ill patients, correlating with higher risks of morbidity and mortality.
Clinical Management
Management involves addressing the root cause:
- Dietary Adjustments: Increased protein intake for malnutrition.
- Medication: Diuretics for edema and managing fluid balance.
- Underlying Disease Management: Treating infections, liver disease, or kidney conditions.
Hyperalbuminemia
Hyperalbuminemia is a rare condition defined by abnormally high levels of albumin in the blood, most commonly caused by dehydration rather than an overproduction of the protein. It is generally asymptomatic, and while often benign, it can occasionally be associated with high-protein diets, severe infections, or metabolic syndrome.
Causes and Associations
- Dehydration: The primary cause, as reduced fluid volume makes the blood more concentrated, increasing the relative concentration of albumin.
- High-Protein Diet/Supplements: Excessive protein intake can contribute to elevated levels.
- Metabolic Syndrome: Associated with insulin resistance, which may trigger increased liver production of albumin.
- Rare Conditions: Severe infections.
Clinical Significance
- Symptoms: Hyperalbuminemia typically causes no direct symptoms on its own.
- Diagnosis: Often discovered during routine blood tests (Comprehensive Metabolic Panel).
- Management: Usually, no extensive workup is required if the patient is otherwise asymptomatic and laboratory findings are normal.
Potential Effects
- Calcium Levels: It can affect the interpretation of calcium tests, often requiring a calculated “corrected calcium” level.
- Liver/Kidney: It is generally not associated with liver or kidney failure, unlike hypoalbuminemia (low albumin), which is associated with serious illness.
Globulin
Globulins are a group of essential proteins produced by the liver and immune system that play critical roles in immune function, blood clotting, and transporting nutrients. Divided into alpha, beta, and gamma types, they are key indicators of health, with normal serum levels typically ranging from 2.0 to 3.5 g/dL.
Key Aspects of Globulin:
- Types and Functions:
- Clinical Significance:
- High Levels: May indicate chronic inflammation, infections, liver diseases, or blood cancers like multiple myeloma.
- Low Levels: Can suggest liver or kidney disease, malnutrition, or immune system deficiencies.
- Testing: Measured via a Total Protein test or Serum Protein Electrophoresis to assess liver/kidney health and immune function.
Globulins, along with albumin, make up the total protein content in blood serum.
Alpha and beta globulins are essential blood proteins synthesized primarily in the liver, functioning mainly as transporters for substances like vitamins, lipids, and iron, as well as acute-phase reactants during inflammation. They are crucial for maintaining colloidal osmotic pressure and, when elevated, can indicate liver disease, chronic infection, or cancer.
Alpha Globulins (α-1 and α-2)
- Functions: Act as transporters (e.g., antitrypsin, haptoglobin, ceruloplasmin) for substances like copper and hemoglobin.
- Significance: Alpha-2 globulins act as acute-phase reactants, increasing during inflammation, tissue damage, or infections.
- Components: Includes alpha-fetoprotein (AFP), which is significant in fetal development and as a tumor marker for liver cancer.
Beta Globulins (β-1 and β-2)
- Functions: Primarily involved in transporting lipids, iron (via transferrin), and hormones.
- Significance: Beta-globulins, such as complement proteins and transferrin, are essential for iron transport and innate immune defense.
- Clinical Relevance: High levels can indicate iron deficiency anemia (due to increased transferrin) or obstructive jaundice.
Gamma globulins, or immunoglobulins (Ig), are essential blood proteins acting as antibodies, produced by B lymphocytes and plasma cells to fight infections. They include IgG, IgM, IgA, IgE, and IgD, which identify and neutralize pathogens. Clinically, these proteins are used for passive immunity, treating immune deficiencies, and managing autoimmune disorders.
Key Aspects of Gamma Globulins:
- Function: Act as the primary defense against pathogens, neutralizing viruses and bacteria.
- Composition: Primarily IgG (approx. 80%), with IgA and IgM.
- Clinical Utility:
- IVIG Therapy: Intravenous gamma globulin (IVIG) is used to boost immunity in patients with primary immunodeficiencies.
- Autoimmune Treatment: Used for conditions like Kawasaki disease, ITP, and Guillain-Barré syndrome.
- Post-Exposure Prophylaxis: Provides temporary protection against infections like hepatitis A or measles.
- Levels: High levels (hypergammaglobulinemia) can indicate chronic inflammation, infections, or multiple myeloma, while low levels (hypogammaglobulinemia) indicate immune deficiencies.
Diagnostic Use
- Serum Protein Electrophoresis (SPEP): Measures globulin levels in the blood.
- High Levels: May indicate infections, cirrhosis, or autoimmune diseases.
- Low Levels: Associated with leukemia or genetic, immune-deficient conditions.
Diagnostic Utility
- Serum Protein Electrophoresis: Separates globulins into fractions to identify specific deficiencies or excesses.
- A/G Ratio: The albumin/globulin ratio helps assess liver and kidney health.
- Clinical Indicators: Elevated alpha/beta levels often signal chronic inflammation, while deficiencies may suggest malnutrition or liver disease.
Albumin/Globulin (A/G) Ratio
The
Albumin/Globulin (A/G) ratio is a blood test, often part of a Comprehensive Metabolic Panel (CMP), that compares albumin (liver-produced protein for fluid balance) to globulin (immune system proteins). A normal ratio is typically 1.1 to 2.5. A low ratio (<1.0) may indicate liver disease, kidney disease, or inflammation, while a high ratio (>2.5) may suggest certain immune disorders or dehydration.
Key Aspects of the A/G Ratio
- Purpose: Assesses liver function, kidney function, and immune system status.
- Normal Range: Generally 1.1 to 2.5, though some labs may use 1.2–2.2.
- Formula:
AlbuminGlobulin.
- Included Tests: The A/G ratio is often part of a Comprehensive Metabolic Panel (CMP).
Interpretation of Results
- Low A/G Ratio (< 1.0 or 1.1):
- High Globulins: Caused by chronic infections, autoimmune diseases, or cancers like multiple myeloma.
- Low Albumin: Caused by liver disease (cirrhosis), kidney disease (nephrotic syndrome), or malnutrition.
- High A/G Ratio (> 2.5):
- Low Globulins: Can indicate genetic conditions or immune system issues.
- High Albumin: Often caused by dehydration.
Common Causes for Abnormal Results
Abnormalities in the A/G ratio can indicate several underlying health conditions, including:
- Liver Disease: Impaired synthesis of albumin.
- Kidney Disease: Loss of protein in the urine.
- Chronic Inflammation or Infection: Overproduction of globulins.
- Multiple Myeloma: A type of blood cancer.
- Malnutrition or Malabsorption: Nutritional deficiencies.
Multiple myeloma
Multiple myeloma is a cancer of the plasma cells, a type of white blood cell that produces antibodies, leading to abnormal protein buildup in the bone marrow, kidney damage, bone destruction, and anemia. Common symptoms include bone pain (especially in the back or ribs), fatigue, weakness, frequent infections, and kidney issues. While there is no cure, treatments include chemotherapy, targeted therapy, and stem cell transplants.
Symptoms of Multiple Myeloma
Many patients are asymptomatic in the early stages, with diagnosis often occurring during routine blood or urine tests. As the disease progresses, symptoms often align with the “CRAB” criteria:
- Calcium elevation (hypercalcemia): Causes constipation, confusion, and extreme thirst.
- Renal insufficiency: Kidney damage due to M-proteins.
- Anemia: Causes fatigue and weakness.
- Bone pain/lesions: Weakened bones, often in the spine or ribs, leading to fractures.
- Other Symptoms: Frequent infections, weight loss, and numbness.
Causes and Risk Factors
The exact cause is unknown, but it begins with a genetic mutation in a single plasma cell that causes it to multiply uncontrollably, crowding out healthy blood cells.
- Age: Most patients are over 65.
- Race: Twice as common in African Americans.
- Gender: Slightly more common in men.
- Precursor Condition: It often develops from a condition called Monoclonal Gammopathy of Undetermined Significance (MGUS).
- Other Factors: Obesity, radiation exposure, and family history.
Diagnosis
- Blood/Urine Tests: To detect monoclonal (M) proteins.
- Bone Marrow Biopsy: To check for high numbers of plasma cells.
- Imaging: X-rays, MRI, or CT scans to identify bone lesions.
Treatment and Prognosis
Multiple myeloma is generally treatable but considered incurable.
- Treatments: Proteasome inhibitors, immunomodulating agents, steroids, chemotherapy, and stem cell transplants.
- Prognosis: The five-year relative survival rate is approximately 62% (based on 2015–2021 US data).
Stages of Multiple Myeloma
Staging is often determined by the Revised International Staging System (R-ISS), which looks at factors like blood levels of
𝛽2-microglobulin, albumin, lactate dehydrogenase (LDH), and cytogenetics.
- Stage I: Lower levels of abnormal markers, less advanced disease.
- Stage II: Intermediate disease progression.
- Stage III: Higher levels of markers, indicating more severe, advanced disease.
Autoimmune diseases
Autoimmune diseases occur when the immune system mistakenly attacks healthy cells, tissues, or organs, causing chronic inflammation and damage. With over 80–100 distinct types affecting various body parts, common symptoms include fatigue, joint pain, skin issues, fever, and digestive problems. Though not curable, they are managed with immunosuppressants, anti-inflammatories, and lifestyle adjustments.
Key Aspects of Autoimmune Disease
- Common Types: Examples include Rheumatoid Arthritis (joints), Type 1 Diabetes (pancreas), Lupus (systemic), Hashimoto’s Thyroiditis (thyroid), Psoriasis (skin), and Crohn’s Disease (bowel).
- Causes & Risk Factors: The exact cause is unknown but involves a mix of genetics, environmental triggers (viruses, chemicals), and immune system dysfunction. Women are more commonly affected, often between ages 15 and 50.
- Symptoms: While varying by disease, common symptoms include chronic fatigue, low-grade fever, joint pain/stiffness, muscle aches, and skin rashes.
- Management: Treatment usually aims to manage symptoms, reduce inflammation, and suppress the overactive immune system, with management often requiring specialists like rheumatologists or endocrinologists.
Some people may have more than one autoimmune disorder at the same time. Common diagnostic methods include blood tests to check for specific markers such as anti-nuclear antibodies (ANA) or inflammatory markers.
 Pathology Training Institute in Bangladesh Best Pathology Training Institute in Bangladesh
Pathology Training Institute in Bangladesh Best Pathology Training Institute in Bangladesh