All Pathology Courses
All Pathology Courses. Mobile Phone 01797522136, 01987073965. All Pathology Courses of HRTD Medical Institute are Pathology Training Course 6 Months, Pathology Training Course 1 Year, Diploma in Pathological Lab Technology 2 Years, Diploma in Pathology Assistant 2 Years, Diploma in Pathological Lab Technology 3 Years, Diploma in Lab Technology 4 Years. All these Pathology Courses are available and running in HRTD Medical Institute.

Location of All Pathology Courses
Location of All Pathology Courses. Mobile Phone Number 01797522136, 01987073965. HRTD Medical Institute, Abdul Ali Madbor Mansion, Metro Rail Piller No. 249, Falpotty Mosjid Goli, Flot No. 11. Mirpur-10 Golchattar, Dhaka-1216.
Pathology Courses Fee in HRTD Medical Institute
Pathology Training Course 6 Months Tk 32500/-
Pathology Training Course 1 Year Tk 62500/-
Diploma in Pathologycal Lab Technology 2 Years Tk 102500/-
Diploma in Pathology Assistant 2 Years Tk 102500/-
Diploma in Pathological Lab Technology 3 Years Tk 152500/-
Diploma in Pathological Lab Technology 4 Years Tk 1,98,500/-
Pathology Courses Admission Fee
6 Month Pathology Training Course Admission Fee Tk 10500/-
1 Year Pathology Training Course Admission Fee Tk 12500/-
2 Years Pathology Course Admission Fee Tk 20500/-
3 Years Pathology Course Admission Fee Tk 25500/-
4 Years Pathology Course Admission Fee Tk 30500/-
Pathology Courses Fee and Payment System
Pathology Training Course 6 Months Tk 32500/-
Admission Fee Tk 10500, Monthly Fee Tk 3000/-,
Exam Fee Tk 4000/-
Pathology Training Course 1 Year Tk 62500/-
Admission Fee Tk 12500/-, Monthly Fee Tk 3500/-,
Exam Fee Tk 4000+Tk 4000= Tk 8000/-
Diploma in Pathological Lab Technology 2 Years Tk 102500/-
Admission Fee Tk 20500/-, Monthly Fee Tk 3000/-,
Exam Fee Tk 2500+Tk 2500 + Tk 2500+ Tk 2500=Tk 10000/-
Diploma in Pathology Assistant 2 Years Tk 102500/-
Admission Fee Tk 20500, Monthly Fee Tk 3000/,
Exam Fee Tk 2500+Tk 2500 + Tk 2500+ Tk 2500=Tk 10000/-
Diploma in Pathological Lab Technology 3 Years Tk 1,52,500/-
Admission Fee Tk 25500/-, Monthly Fee Tk 3000/,
Exam Fee Tk 3000+Tk3000+Tk3000+Tk3000+Tk3000+Tk 4000=Tk19000/-
Diploma in Pathological Lab Technology 4 Years Tk 1,98,500/-
Admission Fee Tk 30500/-, Monthly Fee Tk 3000/-,
Exam Fee Tk 3000X8 Semester=Tk 24000/-
Subjects for Pathology Courses
- Human Anatomy and Physiology
- General Chemistry for Medical Science
- Pharmacology
- Microbiology and Antimicrobial Drugs
- Biochemistry
- Hematology
- General Pathology
- Systemic Pathology
- Clinical Pathology
- Pathology for Medical Practice
- Clinical Microbiology
- Medical Biochemistry
- Hematopathology
- Anatomic Pathology
Practical Class for Pathology Courses
- CBC Test
- Total Count Blood Test
- Differential Count Blood Test (DC)
- Hemoglobin Test
- Erythrocyte Sedimentation Rate (ESR)
- Bleeding Time
- Clotting Time
- Lipid Profile Test
- Kidney Function Test
- Liver Function Test
- Electrolyte Test
- HBsAg Test
- Urine R/E Test
- Stool Test
- Occult Blood Test
- Dengue Test
- Chikongunia Test
Human Anatomy and Physiology for Pathology Courses
Human Anatomy:
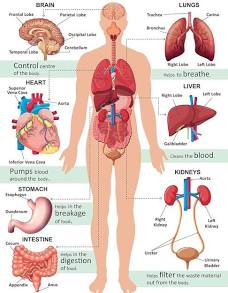

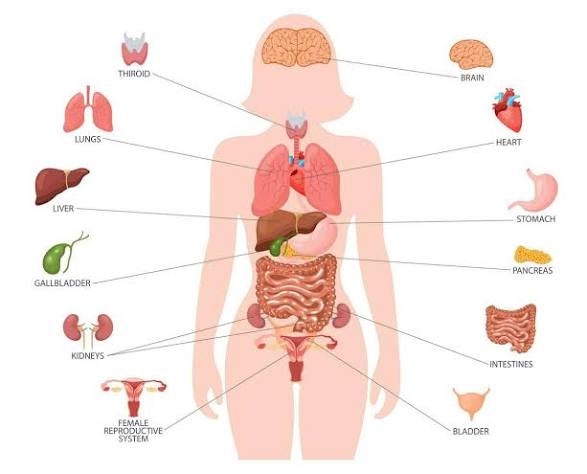
Human Anatomy is the scientific study of the body’s structures, from the microscopic level (cells, tissues) to the macroscopic (organs, systems), focusing on form, location, and relationships between parts, essential for medicine and biology, often studied alongside physiology (how parts function). It’s divided into gross anatomy (visible to the naked eye) and microscopic anatomy (histology/cytology) and explores the body’s eleven major systems, like skeletal, nervous, and circulatory.
Key Branches & Approaches
- Gross Anatomy (Macroscopic): Studying large structures without magnification, through dissection or imaging (X-ray, MRI).
- Microscopic Anatomy (Histology/Cytology): Examining tissues and cells with microscopes.
- Regional Anatomy: Organizing study by body areas (head, limbs, trunk).
- Systemic Anatomy: Organizing by organ systems (e.g., nervous, digestive).
- Radiological Anatomy: Using medical imaging (CT, MRI).
Major Body Systems
- Integumentary: Skin, hair, nails (protection).
- Skeletal: Bones (support, structure).
- Muscular: Muscles (movement, posture).
- Nervous: Brain, spinal cord, nerves (control, coordination).
- Endocrine: Glands, hormones (regulation).
- Cardiovascular (Circulatory): Heart, blood vessels (transport).
- Lymphatic: Lymph nodes, vessels (immunity, fluid balance).
- Respiratory: Lungs, airways (gas exchange).
- Digestive: Stomach, intestines (nutrient absorption).
- Urinary (Excretory): Kidneys, bladder (waste elimination).
- Reproductive: Organs for reproduction.
Human Physiology:
Human physiology is the science of how the human body works, studying its mechanical, physical, and biochemical functions, from cells to organ systems, to maintain a stable internal environment (homeostasis) and respond to challenges like exercise, stress, or disease. It examines systems like nervous, circulatory, respiratory, and digestive, understanding how they interact to keep the body alive and healthy, forming the basis for modern medicine and performance science.
Core Concepts
- Homeostasis: The body’s ability to maintain stable internal conditions (like temperature, pH, blood sugar) despite external changes.
- Levels of Organization: From molecules and cells to tissues, organs, organ systems, and the whole organism.
- Interconnected Systems: Organ systems (e.g., nervous, endocrine, cardiovascular, respiratory) work together, often coordinated by the neuroendocrine system, to achieve body functions.
Key Systems Studied
- Nervous System: Control center, processing signals, thoughts, movements (neurons).
- Endocrine System: Uses hormones to regulate body processes like blood pressure, growth.
- Cardiovascular/Circulatory System: Heart, blood vessels; transports oxygen, nutrients, waste.
- Respiratory System: Lungs, airways; gas exchange (oxygen in, carbon dioxide out).
- Digestive System: Converts food into fuel, absorbing nutrients.
- Urinary System/Renal: Kidneys; maintain blood volume, filter waste.
General Chemistry in Medical Science for Pathology Courses
General Chemistry in Medical Science provides foundational chemical principles (atoms, bonding, reactions, equilibrium, solutions, acids/bases) and links them to biological systems, drug action (pharmacology), and human body processes, covering general, organic, and biochemistry to explain diseases and treatments, crucial for med school prep and understanding medicine at a molecular level.
Core Concepts Covered
- Atomic Structure & Bonding: Understanding elements, isotopes, electron configuration, and how atoms form molecules and interact (like in the body).
- States of Matter & Thermodynamics: How energy and matter change in biological systems (e.g., metabolism).
- Solutions & Acids/Bases: pH balance, buffers, and concentrations in body fluids (blood, etc.).
- Kinetics & Equilibrium: Rates of reactions and reversible processes in cells.
- Electrochemistry: Electron transfer, vital for respiration and nerve signals.
- Organic Chemistry Basics: Carbon compounds, the building blocks of life (carbohydrates, lipids, proteins).
- Biochemistry: Applying chemistry to living organisms, essential for understanding diseases and drugs.
Why It’s Important for Medical Science
- Disease Understanding: Diseases often involve chemical imbalances or dysfunctional molecular interactions.
- Drug Action: Explains how drugs work, their synthesis, and their interaction with the body (Medicinal Chemistry).
- Body Processes: Explains fundamental functions like respiration, nerve impulses, and metabolism.
- Pre-Med/Med School Prep: Serves as a prerequisite for med school and the MCAT, bridging biology and clinical practice.
Pharmacology for Pathology Courses
Pharmacology is the scientific study of drugs (medicines, chemicals, natural substances) and how they interact with living organisms, covering their origins, effects, uses, and toxicity. It explores both pharmacokinetics (how the body processes drugs: Absorption, Distribution, Metabolism, Excretion – ADME) and pharmacodynamics (how drugs affect the body at molecular/cellular levels). This interdisciplinary field bridges basic sciences like biology, chemistry, and physiology to develop new therapies and ensure safe medication use, distinct from the practice of pharmacy (drug dispensing).
Core Areas of Study
- Pharmacokinetics (PK): What the body does to the drug (ADME).
- Pharmacodynamics (PD): What the drug does to the body (mechanism, effects, side effects).
- Drug Discovery & Development: Identifying targets, designing new molecules, testing safety and efficacy.
- Toxicology: Studying the harmful effects of drugs.
- Therapeutic Use: Applying drugs to treat diseases.
Key Concepts
- Drugs: Any substance (natural, synthetic, chemical, biologic) that affects a biological system.
- Receptors: Molecules (often proteins) that drugs bind to initiate effects.
- Pharmacogenetics: How genes influence individual drug responses.
Steroid Drugs, Antibiotic Drugs, Anticholesterol Drugs
Steroid Drugs:
Steroid drugs are medications that mimic naturally occurring hormones and primarily fall into two categories: corticosteroids (used medically to reduce inflammation) and anabolic steroids (used to promote muscle growth, often illicitly).
Corticosteroids
Corticosteroids are synthetic versions of hormones produced by the adrenal glands, such as cortisol. They are powerful anti-inflammatory and immunosuppressant medications used to treat a wide variety of conditions.
Common Uses:
- Inflammatory conditions: Asthma, allergies, rheumatoid arthritis, lupus, inflammatory bowel disease (Crohn’s disease and ulcerative colitis), and multiple sclerosis.
- Skin conditions: Eczema, psoriasis, and other rashes.
- Pain management: As an adjuvant for bone, visceral, and neuropathic pain.
Forms of Administration:
- Oral: Tablets or liquids (e.g., prednisone, dexamethasone) for systemic conditions.
- Inhalers: For respiratory conditions like asthma and COPD.
- Topical: Creams or ointments (e.g., hydrocortisone, mometasone) for skin disorders.
- Injections: Directly into joints, muscles, or the bloodstream for localized or severe inflammation.
Common Examples of Corticosteroid Drugs:
- Prednisone
- Dexamethasone
- Hydrocortisone
- Methylprednisolone
- Betamethasone
Antibiotic Drugs:
Antibiotics are powerful medicines used to treat or prevent infections caused by bacteria. They work by killing bacteria or stopping them from growing and multiplying, but they are not effective against viral infections like colds, the flu, or most sore throats.
Types and Examples of Antibiotics
Antibiotics are generally classified into different groups based on their chemical structure and how they work (their mechanism of action).
| Group | Mechanism of Action | Common Examples | Common Uses |
|---|---|---|---|
| Penicillins | Inhibit cell wall synthesis | Amoxicillin, Penicillin V, Flucloxacillin | Skin, chest, and urinary tract infections, strep throat |
| Cephalosporins | Inhibit cell wall synthesis | Cephalexin, Cefdinir, Ceftriaxone | More serious infections like meningitis, some skin infections |
| Macrolides | Inhibit protein synthesis | Azithromycin, Erythromycin, Clarithromycin | Lung/chest infections (often as a penicillin substitute), pneumonia |
| Tetracyclines | Inhibit protein synthesis | Doxycycline, Minocycline, Tetracycline | Acne, rosacea, Lyme disease, some specific bacterial infections |
| Fluoroquinolones | Inhibit DNA synthesis | Ciprofloxacin, Levofloxacin, Moxifloxacin | Urinary tract infections, respiratory tract infections |
| Aminoglycosides | Inhibit protein synthesis | Gentamicin, Amikacin, Tobramycin | Serious, hospital-only infections (e.g., septicemia) |
| Sulfonamides | Inhibit folic acid synthesis | Trimethoprim-sulfamethoxazole (Bactrim) | UTIs, some types of pneumonia |
Important Considerations
- Prescription Only: Antibiotics are powerful medications that can only be obtained with a prescription from a healthcare provider.
- Follow Instructions: It is crucial to follow the doctor’s instructions carefully and complete the entire course of medication, even if you start feeling better. Stopping treatment early can allow some bacteria to survive, which can lead to a return of the infection or, more seriously, antibiotic resistance.
- Antibiotic Resistance: Overuse or misuse of antibiotics is a major public health concern that leads to bacteria adapting and becoming “superbugs” that existing medicines can no longer treat effectively.
- Side Effects: Common side effects can include nausea, diarrhea, and rash. More serious side effects can occur, including severe allergic reactions or C. difficile infections.
- Alcohol Interaction: While many antibiotics are safe to take with moderate alcohol consumption, certain types, such as metronidazole, can cause severe reactions. Always consult your doctor or pharmacist about potential interactions.
Anticholesterol Drugs:
Anti-cholesterol drugs, primarily Statins (like atorvastatin, rosuvastatin, simvastatin), are first-line treatments that block liver cholesterol production to prevent heart attacks and strokes, but alternatives exist like Ezetimibe, Bempedoic Acid, Fibrates, Bile Acid Sequestrants, and Niacin, often combined with diet and exercise for comprehensive management.
Main Types of Anti-Cholesterol Drugs
- Statins: Most common, reduce the liver’s cholesterol production (e.g., Atorvastatin, Rosuvastatin, Simvastatin).
- Ezetimibe (Zetia): Blocks cholesterol absorption in the intestine; can be used with or without statins.
- Bempedoic Acid (Nexletol): An ATP citrate lyase (ACL) inhibitor, reduces liver cholesterol synthesis, good for those who can’t tolerate statins.
- Fibrates (e.g., Fenofibrate): Primarily lower triglycerides but also affect cholesterol.
- Bile Acid Sequestrants (e.g., Cholestyramine): Bind to bile acids, forcing the body to use cholesterol to make more.
- Niacin (Nicotinic Acid): A B-vitamin in high doses that lowers fats, but has significant flushing side effects.
How They Work
- Statins: block an enzyme in the liver, reducing the amount of cholesterol made.
- Ezetimibe: prevents cholesterol from being absorbed from the gut.
- Fibrates and Niacin affect how the body processes fats (triglycerides and cholesterol).
Biochemistry for Pathology Courses
Biochemistry is the study of chemical processes and substances within living organisms, focusing on life at the molecular level, exploring biomolecules (like proteins, DNA, lipids, carbs) and the reactions that sustain life, energy use, and disease. It blends biology and chemistry, investigating how cells function, communicate, and respond to stimuli, and it forms the foundation for medicine, genetics, agriculture, and biotechnology by explaining the molecular basis of biological functions and malfunctions.
Core Concepts
- Biomolecules: Understanding the structure, function, and interactions of essential molecules like proteins (enzymes), nucleic acids (DNA/RNA), carbohydrates, and lipids.
- Metabolism: The network of chemical reactions (anabolic/building and catabolic/breaking down) that convert food into energy and cellular components, orchestrated by enzymes.
- Molecular Mechanisms: How genes are expressed, cells communicate, and how these processes are regulated.
Key Areas & Applications
- Medicine: Explaining disease causes (e.g., genetic mutations), drug action, and developing treatments.
- Genetics: The chemical basis of heredity, including DNA structure and function.
- Nutrition: How organisms obtain and use nutrients for survival.
- Biotechnology & Agriculture: Developing new bio-based solutions and improving crops.
Branches of Biochemistry:
Biochemistry branches into core areas like Structural Biochemistry, Enzymology, and Metabolism, studying biomolecule shapes, enzyme function, and chemical reactions in life, respectively, while also expanding into fields like Molecular Biology, Genetics, Neurochemistry, Immunology, Clinical Biochemistry, Bioorganic Chemistry, and Biotechnology, focusing on cell processes, heredity, nervous system chemistry, immune responses, medical applications, drug design, and technological uses of biological systems.
Core Branches
- Structural Biochemistry: Focuses on the 3D structure of macromolecules (proteins, DNA, RNA) and their interactions.
- Enzymology: Studies the mechanisms, kinetics, and function of enzymes, the catalysts of life.
- Metabolic Biochemistry: Explores the chemical pathways (metabolism) that sustain living organisms.
- Molecular Genetics/Molecular Biology: Investigates the biochemistry of genes, DNA, RNA, and protein synthesis.
Applied & Specialized Branches
- Clinical Biochemistry: Applies biochemical principles to diagnose and treat diseases.
- Neurochemistry: Studies the chemistry of the nervous system, neurotransmitters, and neurological disorders.
- Immunochemistry/Immunology: Focuses on the molecular basis of immune responses.
- Bioorganic Chemistry: Blends organic chemistry with biology, crucial for drug development and understanding biological mechanisms.
- Biotechnology: Uses biological systems for technological applications, including genetic engineering.
- Toxicology: Studies harmful substances (xenobiotics) on living organisms.
- Plant & Animal Biochemistry: Focuses on the unique biochemistry of plants and animals, including photosynthesis and animal systems.
- Nutritional Biochemistry: Studies the chemical processes of nutrients and diet.
Hematology for Pathology Courses
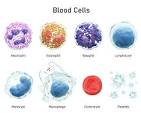
Hematology is the branch of medicine focused on studying blood, blood-forming organs (like bone marrow), and blood diseases, encompassing the causes, diagnosis, treatment, and prevention of conditions affecting red cells, white cells, platelets, and clotting factors. Specialists, called hematologists, diagnose and manage disorders from anemias and infections to leukemia, bleeding disorders (hemophilia, thrombosis), and blood cancers, often combining training with oncology.
What Hematology Covers
- Blood Components: Red blood cells (oxygen transport), white blood cells (immune function), platelets (clotting), and plasma (fluid, proteins).
- Blood-Forming Organs: Bone marrow, lymph nodes, spleen, and thymus.
- Key Conditions:
- Anemias: Iron deficiency, sickle cell disease.
- Cancers: Leukemia, lymphoma, multiple myeloma.
- Clotting Disorders: Hemophilia, deep vein thrombosis (DVT), and immune thrombocytopenia (ITP).
- Infections: Managing blood-related infections.
What Hematologists Do
- Diagnosis: Using blood tests, bone marrow biopsies, and other evaluations.
- Treatment: Administering chemotherapy, immunotherapy, transfusions, and other therapies.
- Consultation: Working with other doctors to manage blood issues in various illnesses.
Types of Specialists
- Hematologist: Focuses on direct patient care for blood disorders.
- Hematopathologist: A pathologist who studies blood and bone marrow diseases in a lab setting.
- Hematology-Oncology: A combined specialty for blood cancers and other cancers.
Hematopathology for Pathology Courses
Hematopathology is the pathology subspecialty focused on diagnosing diseases of the blood, bone marrow, and lymphoid tissues (like lymph nodes), examining blood cells (red, white, platelets) and their origins, using tools like microscopy, flow cytometry, and molecular tests to identify conditions like leukemia, lymphoma, anemias, and bleeding disorders. Hematopathologists integrate complex lab data to provide accurate diagnoses, often working closely with hematologist-oncologists.
What Hematopathologists Study & Diagnose
- Blood Cells: Red cells, white cells, platelets, and their disorders (e.g., anemia, clotting issues).
- Lymphatic System: Lymph nodes, spleen, thymus, and related cancers (lymphoma, leukemia).
- Bone Marrow: Disorders affecting blood cell production (e.g., myelodysplastic syndromes, myeloproliferative disorders).
Key Diagnostic Tools & Techniques
- Microscopy: Examining blood smears, bone marrow, and tissue biopsies.
- Flow Cytometry: Analyzing cell surface markers to identify and quantify cell populations.
- Immunohistochemistry (IHC): Using antibodies to stain cells for specific proteins.
- Molecular Testing: DNA sequencing and cytogenetics for genetic abnormalities (e.g., gene mutations, chromosomal changes).
Why It’s Important
- It bridges basic lab tests (like CBCs) with advanced analysis to understand complex hematologic conditions.
- Accurate diagnosis is crucial for guiding targeted therapies for blood cancers and other serious disorders.
General Pathology for Pathology Courses
General Pathology studies the fundamental mechanisms of disease, focusing on how cells, tissues, and organs respond to injury, leading to structural and functional changes, and involves diagnosing illnesses through lab tests like biopsies, blood analysis, and advanced imaging to understand the “why” and “how” of disease for patient care. It covers basic cellular responses (inflammation, adaptation, repair) and broad disease processes (infections, cancers) before branching into specific areas such as surgical or molecular pathology, serving as a bridge between basic science and clinical medicine.
Core Concepts
- Cellular Injury & Adaptation: How cells cope with stress (e.g., hypertrophy, atrophy, metaplasia) or die (necrosis).
- Inflammation & Repair: The body’s response to damage, including blood vessel changes (hyperemia) and wound healing.
- Disorders of Growth: Neoplasia (cancer) and other abnormal cell proliferation (hyperplasia).
- Biochemical Disturbances: Fatty changes (steatosis) or glycogen accumulation in tissues.
- Infectious Diseases: How pathogens like viruses (HPV causing warts) or parasites (tapeworms causing cysticercosis) cause illness.
Key Areas & Tools
- Sub-disciplines: Anatomical Pathology (tissues, biopsies), Clinical Pathology (blood, fluids), Surgical Pathology, Forensic Pathology, Molecular Pathology, etc.
- Diagnostic Techniques: Microscopy (light, electron), biopsies, blood tests, PCR, sequencing, special stains.
Role of a Pathologist
- Diagnosis: Using lab findings to identify diseases.
- Consultation: Advising other doctors on treatment.
- Broad Scope: Managing a diverse range of cases, from common infections to complex cancers.
Systemic Pathology for Pathology Courses
Systemic pathology is the branch of medicine that studies diseases as they affect specific organs and body systems (like heart, lungs, kidneys), focusing on etiology (causes), pathogenesis (development), morphological changes, and the resulting clinical signs, serving as a bridge between general disease principles (General Pathology) and clinical practice. It explains why a disease happens in a particular system (e.g., H. pylori in the stomach), how it progresses, and its effects on the body, integrating cellular responses with organ function.
Key Components
- Etiology: The study of disease causes (e.g., bacteria, genetics, lifestyle).
- Pathogenesis: The sequence of events from the initial cause to the final disease manifestation.
- Morphological Changes: Alterations in cells, tissues, and organs (microscopic/histopathological and gross appearance).
- Clinical Manifestations: How the disease presents as signs and symptoms in patients.
Clinical Pathology
Clinical pathology, also known as laboratory medicine, diagnoses diseases by analyzing bodily fluids (blood, urine, and spinal fluid) and tissues using chemistry, microbiology, hematology, and molecular techniques, acting as a vital link between lab tests and patient care to guide treatment. Clinical pathologists oversee these labs, ensuring quality and interpreting results to help doctors manage patient health, covering areas from basic blood counts to complex genetic testing.
Key Aspects of Clinical Pathology
- Tests Samples: Analyzes blood, urine, cerebrospinal fluid, joint fluid, bone marrow, and other specimens.
- Broad Disciplines: Includes clinical chemistry, hematology (blood disorders), clinical immunology, and molecular pathology.
- Supports Diagnosis: Provides data for diagnosing, monitoring, and preventing diseases, impacting many healthcare decisions.
- Laboratory Focus: Different from anatomic pathology (which examines tissues/organs directly), clinical pathology focuses on the biochemical and cellular components within fluids.
- Professional Role: Involves medical doctors (pathologists) and scientists who manage testing, quality control, and interpret complex results, working with physicians.
Pathology for Medical Practice
Pathology for Medical Practice is the crucial bridge between basic science and clinical care, focusing on the study of disease to aid in diagnosis, treatment, and management, involving examination of tissues (Anatomic Pathology) and body fluids (Clinical Pathology). It underpins most medical decisions, from cancer diagnosis and genetic testing to infectious disease identification, using methods like microscopy, molecular testing, and lab analysis to understand disease causes and effects, ultimately guiding personalized patient care.
Key Aspects of Pathology in Practice:
- Diagnosis: Identifying diseases by examining cells, tissues (biopsies), blood, and other fluids for abnormalities.
- Treatment Guidance: Providing critical information for oncologists (cancer type/stage), infectious disease specialists (microbes/antibiotics), and others to develop treatment plans.
- Monitoring: Tracking disease progression and response to therapy.
- Prevention: Identifying predispositions and risk factors through advanced molecular testing.
Branches of Pathology:
- Anatomic Pathology: Studies disease at the tissue/cellular level (biopsies, cytology, autopsies).
- Clinical Pathology (Laboratory Medicine): Involves Hematology, Immunology, Microbiology, and Clinical Chemistry.
- Molecular Pathology: Uses genetic/biomolecular analysis for personalized medicine, vital for cancer and infections.
- Forensic Pathology: Determines the cause of death in legal contexts (e.g., autopsies).
Role in Medical Practice:
- Support Specialty: Acts as a core support for all other clinical staff, with over 70% of healthcare decisions involving pathology.
- Bridging Science & Medicine: Connects laboratory findings to patient care, informing decisions from initial diagnosis to ongoing management.
- Patient-Centered: Every lab result or tissue analysis directly impacts a patient’s care, making it central to modern healthcare.
Anatomic Pathology for Pathology Courses
Anatomic pathology is a medical specialty focused on diagnosing diseases by examining organs, tissues, and cells (biopsies, surgical samples, bodily fluids) under a microscope, using techniques like histopathology (tissues), cytology (cells), and molecular tests to see structural changes, guiding treatment, and sometimes performing autopsies. It’s the scientific foundation of medicine, helping doctors understand disease causes, monitor patients, and contribute to research.
Key Areas & Procedures
- Histopathology: Microscopic study of preserved tissue samples (biopsies, surgical resections).
- Cytology: Examination of individual cells, such as from Pap smears or fine needle aspirations.
- Gross Examination: Visual inspection and description of large specimens.
- Special Stains & Immunohistochemistry (IHC): Using antibodies and dyes to highlight specific cellular components or markers (e.g., tumor types).
- Molecular Pathology: Analyzing DNA and RNA for genetic mutations, crucial for personalized medicine.
- Autopsy Pathology: Investigating the cause and manner of death, often for clinical education or forensic purposes.
What They Do
- Diagnose: Identify cancers, infections, inflammatory conditions, and genetic disorders.
- Guide Treatment: Provide essential diagnoses for surgeons, oncologists, and other specialists.
- Research: Contribute to understanding disease mechanisms and developing new therapies.
- Consult: Act as “doctor’s doctors,” working with other clinicians to solve complex cases.
Subspecialties
- Dermatopathology: Skin diseases.
- Neuropathology: Nervous system diseases.
- Gastroenterology Pathology: Digestive system diseases.
- Hematopathology: Blood and blood-forming organs.
Clinical Microbiology
Clinical microbiology is the medical specialty focused on identifying microorganisms (bacteria, viruses, fungi, parasites) causing infections in humans to aid in diagnosis, treatment, and prevention, using lab techniques like culturing, staining, molecular tests, and serology, playing a crucial role in patient care and public health.
Core Functions
- Diagnosis: Identifying pathogens in patient samples (blood, urine, swabs).
- Treatment Guidance: Determining effective antibiotics or antivirals (antimicrobial susceptibility testing).
- Infection Control: Monitoring and preventing outbreaks.
- Consultation: Advising clinicians on testing and infection management.
Key Techniques Used
- Microscopy & Staining: Gram stain for initial bacterial identification.
- Culture: Growing microbes on agar plates for isolation and identification.
- Molecular Methods: PCR, DNA sequencing for rapid and precise pathogen detection.
- Immunology: Antigen/antibody tests (serology).
- Automation: Automated systems for high-throughput processing.
Importance
- Patient Outcomes: Guides therapy, reduces antibiotic resistance.
- Public Health: Detects emerging pathogens and controls epidemics.
- Dynamic Field: Constantly evolving with new technologies like genomics and automation.
CBC Test
A CBC (Complete Blood Count) is a common blood test that checks your overall health by measuring and analyzing the different cells in your blood: red blood cells (oxygen transport), white blood cells (infection fighting), and platelets (clotting). It helps diagnose conditions like anemia, infections, inflammation, or leukemia, and monitors existing treatments, usually involving a simple blood draw from a vein.
What it measures
- White Blood Cells (WBC): Fights infection (total count and differential types).
- Red Blood Cells (RBC): Carries oxygen (count, Hemoglobin, Hematocrit, size/indices like MCV).
- Platelets: Help blood clot.
- Hemoglobin (Hb): Oxygen-carrying protein in RBCs.
- Hematocrit (Hct): Proportion of blood volume made of RBCs.
Why is it done
- Part of routine checkups.
- Investigate symptoms like fatigue, fever, bruising, or weakness.
- Monitor chronic diseases (e.g., kidney disease, cancer).
- Check response to treatments or medications.
How it’s done
- A nurse draws a small blood sample from a vein, usually in your arm.
- The sample is analyzed by an automated machine.
- Results compare your levels to normal ranges, flagging any highs or lows.
Total Count Blood Test (TC)
A “total count blood test” usually refers to a Complete Blood Count (CBC), a common panel that measures the types and numbers of cells in your blood (Red Blood Cells, White Blood Cells, Platelets), plus key metrics like Hemoglobin and Hematocrit, to check overall health, diagnose conditions like anemia or infection, and monitor treatments, by analyzing if cell levels are too high (infection/inflammation) or low (bleeding/bone marrow issues).
What it measures:
- Red Blood Cells (RBCs): Carry oxygen. (Count, Hemoglobin, Hematocrit).
- White Blood Cells (WBCs): Fight infection (Count, plus a “Differential” to see types: Neutrophils, Lymphocytes, etc.).
- Plate00
- .
- lets (PLTs): Help blood clot (Count, Mean Platelet Volume).
Why it’s done:
- Detects infections, anemia, inflammation, and bleeding disorders.
- Checks general health and monitors chronic diseases.
- Evaluates symptoms like fatigue, weakness, or bruising.
How it works:
- A healthcare professional takes a blood sample from a vein in your arm.
- The lab counts the cells and measures other components.
What results mean (briefly):
- High WBC: Might mean infection or inflammation.
- Low Hemoglobin/RBC: Often anemia.
- High/Low Platelets: Can relate to clotting issues or bone marrow problems.
Clinical Procedure for Total Count Blood Test (TC)
The Total Count (TC) blood test, which is part of a Complete Blood Count (CBC), is a simple procedure involving a standard blood draw (venipuncture) performed by a healthcare professional. The sample is then analyzed in a laboratory to measure the total number of white blood cells (leukocytes) in your blood.
Preparation for the TC Blood Test
Generally, no specific preparation is required for a TC blood test.
- Fasting is usually not necessary unless your doctor has ordered additional tests on the same blood sample that require it (such as a cholesterol test).
- Medication: Inform your healthcare provider about all medications, supplements, or recent medical treatments (like chemotherapy or radiation) you are taking, as some can affect the results. Your doctor may advise you to stop certain medications temporarily.
- Clothing: Wear a short-sleeved shirt or a shirt with sleeves that can be easily rolled up to provide easy access to your arm.
Procedure for the TC Blood Test
The procedure is quick and is typically performed by a phlebotomist (a healthcare professional trained in drawing blood) in a clinic, hospital, or lab setting.
- Site Selection and Cleaning: The technician will select a vein, usually from the inside of your elbow or the back of your hand. They will clean the area with an antiseptic wipe to prevent infection.
- Tourniquet Application: An elastic band (tourniquet) is placed around your upper arm to make the vein swell with blood and become more visible.
- Blood Collection: A sterile needle connected to a collection tube is inserted into the vein. You may feel a brief sting or pinch when the needle is inserted.
- Sample Collection: A small amount of blood is collected into one or more vials.
- Bandaging: After the required amount of blood is drawn, the elastic band and needle are removed, and a bandage or cotton pad is applied to the puncture site to stop any bleeding.
- Lab Analysis: The collected sample is labeled and sent to a laboratory for analysis, often using automated analyzers to count the white blood cells.
Post-Procedure and Results
After the test, you can usually return to your normal daily activities right away. There is minimal risk, with slight pain or bruising at the needle insertion site being the most common side effects.
Results are typically available within hours to a day and should be discussed with your healthcare provider for proper interpretation and diagnosis. The normal range for a total white blood cell count in adults is generally between 4,000 and 11,000 cells per microliter of blood, but range can vary slightly by laboratory.
Differential Count Blood Test (DC)
A Differential Count (DC) blood test, often part of a Complete Blood Count (CBC), provides a detailed breakdown of the different types of white blood cells (WBCs)—neutrophils, lymphocytes, monocytes, eosinophils, and basophils—to assess immune function, diagnose infections, inflammation, allergies, and blood disorders like leukemia, by revealing percentages and absolute numbers of each cell type, which helps identify issues beyond a simple WBC count.
What it measures
The test quantifies the five main types of WBCs:
- Neutrophils: Fight bacterial infections.
- Lymphocytes (B & T cells): Target viruses, cancer cells, and produce antibodies.
- Monocytes: Remove pathogens and dead cells.
- Eosinophils: Combat parasites and manage allergic reactions.
- Basophils: Release enzymes during allergic responses.
Why is it done
- Diagnose Infections & Inflammation: Identify bacterial (high neutrophils) or viral (high lymphocytes) issues.
- Detect Allergic Reactions: High eosinophils suggest allergies or parasites.
- Monitor Immune Disorders: Assess conditions like autoimmune diseases or HIV.
- Screen for Blood Cancers: Detect abnormal WBCs or blasts.
- Evaluate Symptoms: Investigate fatigue, unexplained bruising, or frequent infections.
How it works
- A blood sample is taken, often as part of a CBC.
- A lab technician examines a blood smear under a microscope or uses automated analyzers.
- They count and classify 100-200 WBCs, noting percentages.
- These percentages are multiplied by the total WBC count (from the CBC) to get absolute counts, which are more informative than percentages alone.
What results mean
- High Counts: Can indicate infection, inflammation, stress, or certain diseases.
- Low Counts: May signal a weakened immune system, bone marrow issues, or damage from treatments like chemotherapy.
- Abnormal Ratios: Reveal specific problems, like an excess of immature cells pointing to leukemia.
Clinical Procedure for Differential Count Blood Test (DC)
The clinical procedure for a Differential Count (DC) blood test involves two main stages: blood sample collection and laboratory analysis. Analysis can be performed using either automated analyzers or a manual microscopic method.
I. Sample Collection (Phlebotomy)
No special preparation, such as fasting, is usually required for a DC test.
- A healthcare professional, such as a phlebotomist, will typically draw a blood sample from a vein in the inside of your elbow or the back of your hand. For infants, a heel prick may be used.
- The skin is cleaned with an antiseptic wipe.
- An elastic band (tourniquet) is placed around the upper arm to make the vein swell with blood and easier to access.
- A sterile needle is inserted into the vein, and a small amount of blood is collected into a test tube or vial, typically one with a purple or lavender top containing the anticoagulant EDTA to prevent clotting.
- The tourniquet is removed, the needle is withdrawn, and a bandage is applied to the puncture site to stop any bleeding.
II. Laboratory Analysis
Once in the lab, the sample is processed to identify and count the five major types of white blood cells (WBCs): neutrophils, lymphocytes, monocytes, eosinophils, and basophils.
A. Automated Differential Count
Most differentials are performed using automated hematology analyzers, which are faster and more accurate than manual methods for general screening.
- The machine uses methods like fluorescence flow cytometry, electrical impedance, and light scatter to analyze thousands of cells and categorize them by size, shape, and internal properties.
- The results are typically reported as both percentages and absolute counts.
- If the automated system detects abnormal results, the sample is flagged for a manual review by a trained laboratory specialist.
B. Manual Differential Count (Microscopic Review)
A manual count is performed when an automated test shows unusual results or when a physician specifically requests it.
- Smear Preparation: A drop of the blood sample is thinly spread across a glass slide to create a blood film and allowed to air dry.
- Staining: A special dye, usually a Romanowsky stain like Wright’s or Giemsa stain, is applied to the smear. The stain helps differentiate the various cell types based on their morphology, including nuclear features and cytoplasmic granules.
- Microscopic Examination: A trained laboratory specialist examines the stained slide under a microscope, using oil immersion (1000x magnification) if necessary, to identify cells based on their appearance.
- Counting and Classification: The specialist systematically scans a specific area of the smear, counting and classifying at least 100 white blood cells.
- Reporting: The counts are recorded (often using a manual counter) and converted into percentages and absolute values. The report may also note any abnormal or immature cells.
 Pathology Training Institute in Bangladesh Best Pathology Training Institute in Bangladesh
Pathology Training Institute in Bangladesh Best Pathology Training Institute in Bangladesh